David R. Meldrum, MD
 The Meldrum quads
The Meldrum quads
People have often asked whether it makes me more conservative in managing infertile couples to have had quadruplets myself. There’s no simple answer, but that’s probably somewhat true. Everyone who gets through a multiple pregnancy without a major complication should be very thankful. Twins usually do well, and no question, it’s “two for the price of one”. But even twins can be delivered early enough so one or both offspring doesn’t survive or could have a major impairment such as cerebral palsy, brain damage, or other major or minor handicap.  Twins are also a major stress for your relationship and divorce has been shown to occur more often. When all of the pluses and minuses are considered, it’s actually better to undergo more expense to have each baby one at a time. Recent studies have even shown that when more than one embryo is transferred and a second sac shrinks away, or even if there is no sign of another implantation, a resulting singleton pregnancy will have more complications than when only one embryo is transferred. This is presumably because of inflammation associated with another implantation that fails to develop. It is also why it is not a good strategy to add a poor embryo to the transfer just because it formed and would otherwise be discarded. It could cause complications of a pregnancy resulting from the good quality embryo.
Twins are also a major stress for your relationship and divorce has been shown to occur more often. When all of the pluses and minuses are considered, it’s actually better to undergo more expense to have each baby one at a time. Recent studies have even shown that when more than one embryo is transferred and a second sac shrinks away, or even if there is no sign of another implantation, a resulting singleton pregnancy will have more complications than when only one embryo is transferred. This is presumably because of inflammation associated with another implantation that fails to develop. It is also why it is not a good strategy to add a poor embryo to the transfer just because it formed and would otherwise be discarded. It could cause complications of a pregnancy resulting from the good quality embryo.
So how can you have one embryo transferred and still keep your success rate high and the process as efficient as possible? First, for women under age 35, transfer of a single day 5 embryo (a blastocyst) of good quality will give a high chance of pregnancy. With current cryopreservation by vitrification the survival of that additional embryo will be so high that your overall success rate will be unchanged. You just have to accept a bit higher chance of having to undergo the inconvenience and expense of transfer of that second embryo.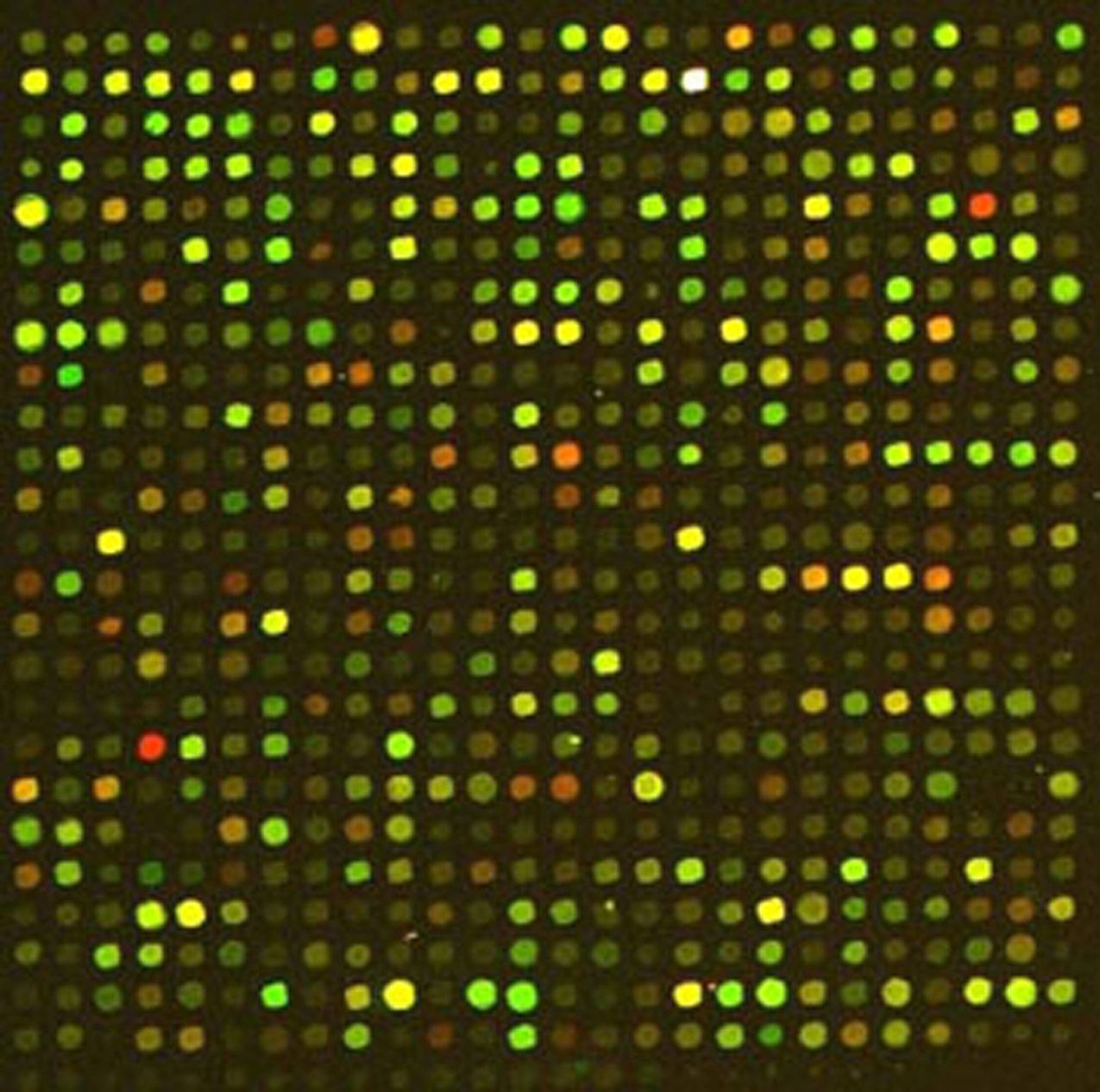 For women over age 35 and particularly over age 38, you can have a single embryo transferred while maintaining a high chance of pregnancy, but it requires additional expense and an adjustment of expectations and some patience. It can be accomplished by sampling each embryo on day 5 to verify that all chromosomes are normal using many thousands of genetic probes, followed by cryopreservation and transfer of a single normal embryo in a later cycle. By transferring only chromosomally normal embryos the process becomes much more efficient, requiring fewer embryo transfers. Transferring in a cycle where the endometrium has not been stimulated has recently been shown to also result in a higher chance of implantation.
For women over age 35 and particularly over age 38, you can have a single embryo transferred while maintaining a high chance of pregnancy, but it requires additional expense and an adjustment of expectations and some patience. It can be accomplished by sampling each embryo on day 5 to verify that all chromosomes are normal using many thousands of genetic probes, followed by cryopreservation and transfer of a single normal embryo in a later cycle. By transferring only chromosomally normal embryos the process becomes much more efficient, requiring fewer embryo transfers. Transferring in a cycle where the endometrium has not been stimulated has recently been shown to also result in a higher chance of implantation.  The technique is called “trophectoderm biopsy”, meaning that a small hole is made in the egg shell using a laser, and when cells destined to become the placenta start hatching, a few cells are trimmed off, again using the laser. The cells are then sent to a special lab to determine whether every chromosome is normal. (Incidentally, that also will tell you which of the embryos will be boys or girls.) The chance of miscarriage, which is usually due to a chromosome abnormality, will be lower.
The technique is called “trophectoderm biopsy”, meaning that a small hole is made in the egg shell using a laser, and when cells destined to become the placenta start hatching, a few cells are trimmed off, again using the laser. The cells are then sent to a special lab to determine whether every chromosome is normal. (Incidentally, that also will tell you which of the embryos will be boys or girls.) The chance of miscarriage, which is usually due to a chromosome abnormality, will be lower. 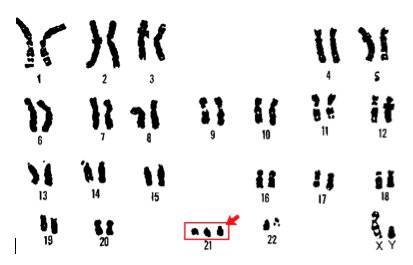 As well, the chance of an ongoing pregnancy being chromosomally abnormal, such as Down’s syndrome, where there is an extra chromosome 21 (right), will also be much lower, reducing the chance of needing a pregnancy termination or having a chromosomally abnormal newborn. However, even with the excellent techniques used today, you should still realize that the chance of a chromosomally abnormal fetus is not reduced to zero, because the technique is not perfect. Also, there is a very small chance that the sex determination could be wrong. However, if you factor in the lower risk of pregnancy complications and miscarriage (understanding that those are generally covered by your insurance), the additional expense (about $6,000) is easily justified. It is unfortunate that insurance doesn’t cover both infertility and these other medical costs.
As well, the chance of an ongoing pregnancy being chromosomally abnormal, such as Down’s syndrome, where there is an extra chromosome 21 (right), will also be much lower, reducing the chance of needing a pregnancy termination or having a chromosomally abnormal newborn. However, even with the excellent techniques used today, you should still realize that the chance of a chromosomally abnormal fetus is not reduced to zero, because the technique is not perfect. Also, there is a very small chance that the sex determination could be wrong. However, if you factor in the lower risk of pregnancy complications and miscarriage (understanding that those are generally covered by your insurance), the additional expense (about $6,000) is easily justified. It is unfortunate that insurance doesn’t cover both infertility and these other medical costs.  In some countries in Europe the government mandates the transfer of a single embryo under most circumstances with initial IVF attempts, realizing that the overall cost will be lower. We do understand that when IVF expenses are out of pocket, as is often the case in this country and the expenses for complications are covered by insurance, couples can be swayed toward transferring more embryos. Still, to my mind, the decision is trumped by reducing the chance, however unlikely, of having a seriously impaired offspring, with the obvious lifelong difficulties and expense.
In some countries in Europe the government mandates the transfer of a single embryo under most circumstances with initial IVF attempts, realizing that the overall cost will be lower. We do understand that when IVF expenses are out of pocket, as is often the case in this country and the expenses for complications are covered by insurance, couples can be swayed toward transferring more embryos. Still, to my mind, the decision is trumped by reducing the chance, however unlikely, of having a seriously impaired offspring, with the obvious lifelong difficulties and expense.
Even in women anticipated to have a low response”, we have found that this same strategy is effective. That may be because we routinely use clomiphene citrate (CC) as part of the stimulation regimen. CC may enhance the quality of the embryos in such women.
So, in summary, if you are under 35 and have good quality blastocysts, you should strongly consider single embryo transfer. If you are over 35, you can consider testing of each embryo on day 5 and transfer of a single normal embryo after cryopreservation, either as an initial approach or if routine IVF is not successful. To make the process more efficient, some women under age 35 will chose to have chromosome testing because of the likely formation of several embryos. We have had repeated singleton pregnancies in such women with transfers of single chromosomally normal embryos. Otherwise, it could require many more embryo transfers.
 I did mention sex selection, which deserves further comment. Because on average half of the embryos will be of the “deselected” sex, and usual success rates are based on being able to choose the best embryo/s from all available embryos, sex selection will reduce your chance of success (let’s estimate that effect as a one-third decrease until enough data are gathered). For couples with normal fertility the reduction might be small and not significant, but for a couple struggling with infertility, any sizable reduction probably won’t be tolerable. Of course there are variations on that decision. A couple could decide if there are two embryos of equal quality to try transferring the desired sex first. Or they could transfer each reasonable embryo of the desired sex followed later by the initially deselected sex if they are unsuccessful.
I did mention sex selection, which deserves further comment. Because on average half of the embryos will be of the “deselected” sex, and usual success rates are based on being able to choose the best embryo/s from all available embryos, sex selection will reduce your chance of success (let’s estimate that effect as a one-third decrease until enough data are gathered). For couples with normal fertility the reduction might be small and not significant, but for a couple struggling with infertility, any sizable reduction probably won’t be tolerable. Of course there are variations on that decision. A couple could decide if there are two embryos of equal quality to try transferring the desired sex first. Or they could transfer each reasonable embryo of the desired sex followed later by the initially deselected sex if they are unsuccessful.
So how did the Meldrum quads do? They delivered at 34 weeks and did well. It was certainly very difficult, but Claudia is incredibly well-organized and our marriage was strengthened by all of the challenges. However, I have seen enough instances over the years where things did not go well that we consider ourselves extremely fortunate.

